Optical impressions in odontology
13 January 2025CAD/CAM: an essential partner in modern dentistry
15 January 2025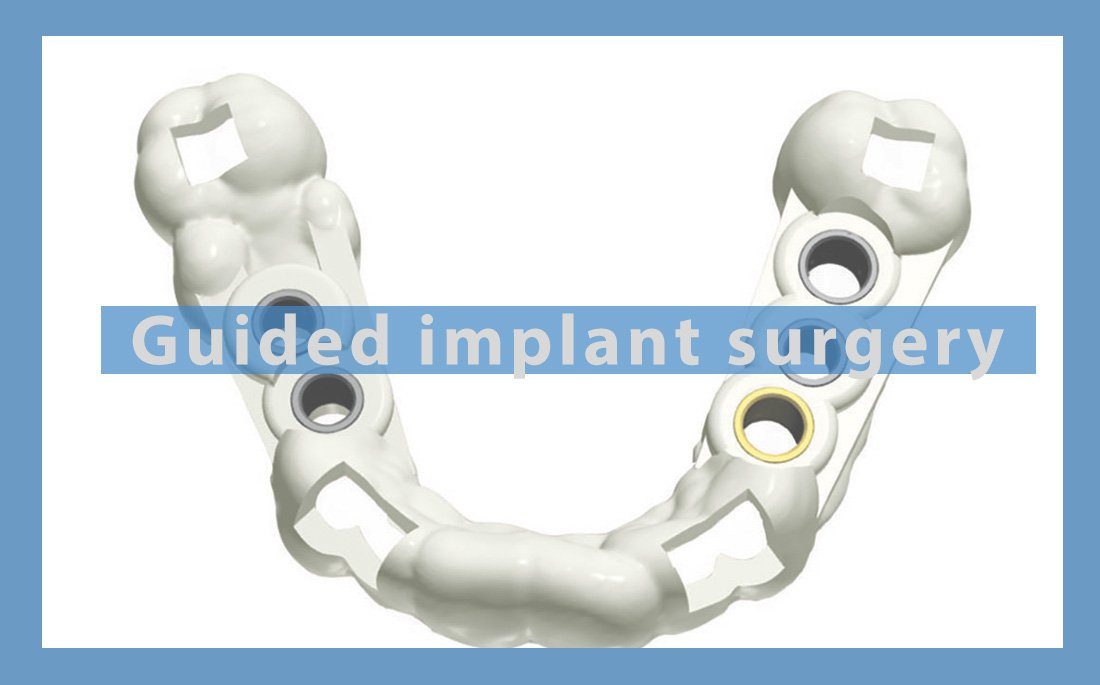
Guided implant surgery
Over the last few years, the trio of modern implantology development, imaging techniques and the digital revolution have combined to spawn the growth of a new protocol: computer aided implantology (CAI), or guided implant surgery.
This innovative technique is used to fit dental implants using a digitally made guide, without disrupting the basic rule of modern implantology, where the prosthetic project controls the position of the implant and therefore the surgery.
The primary aim of this surgical technique is to help the implantologist to preserve maxillary anatomical structures, but it also enables them to conduct an instant aesthetic procedure that is less invasive.
This article will talk briefly about the history of guided implantology, its principle, the various stages of the protocol, the technique of guide manufacturing. You will also discover its advantages and limitations, including a look at the various concepts and systems currently available, as well as the various types of possible guides.
A brief history for guided implant surgery
The very first guides date back to 1999, and were bone-supported. Invasive surgery with flaps was therefore necessary to direct the guide into the right position on the bone. After lifting the flap, the inner surface of the guide was adjusted and stabilised directly on the bone.
These guides were made using 3D bone reconstruction techniques, by converting DICOM radiological files into .STL files. The first beneficiary of guided surgery was therefore the fully edentulous patient, because of the problems encountered with radiological guides used during this era.
The idea was to simplify complex and invasive surgeries.
A few years later, in 2002, the mucosa-supported surgical guide was developed, thanks to the use of a radiopaque palate that defined the volume of soft tissue. The double scanning technique was used to produce mucosa-supported guides for flapless surgery. As its name indicates, this technique can be used to avoid lifting a flap and use a trans-gingival procedure.
Thanks to tomodensitometric X-Rays (Scanner and Cone beam), we can differentiate bony areas from soft tissues. The inner surface of the imaging guide can be used to accurately model the surgical guide.
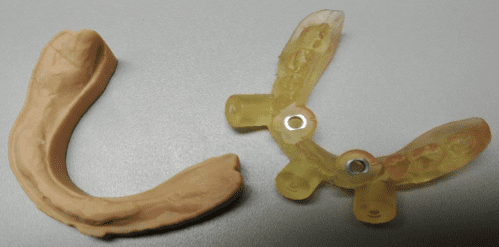
Figure 1 Mucosa-supported stereolithographic surgical guide
Latest generation guides are now made using digital laboratory models, while the latest advance involves using intra-buccal optical impressions to design the surgical guide.
Guided implant surgery is now used to treat partially edentulous patients.
The Principle
Guided implant surgery uses a planning software that enables “matching”, or the overlaying of radiological (DICOM file) and clinical (.STL file) patient data. DICOM files are generated by a Cone Beam X-Ray or scanner. .STL files are generated by digital impressions of the patient’s mouth.
Overlaying all of these digital files can be done automatically or manually.
Matching aims to synchronise radiological data with tooth and gingival surfaces that the inner surface of the guide will be placed on.
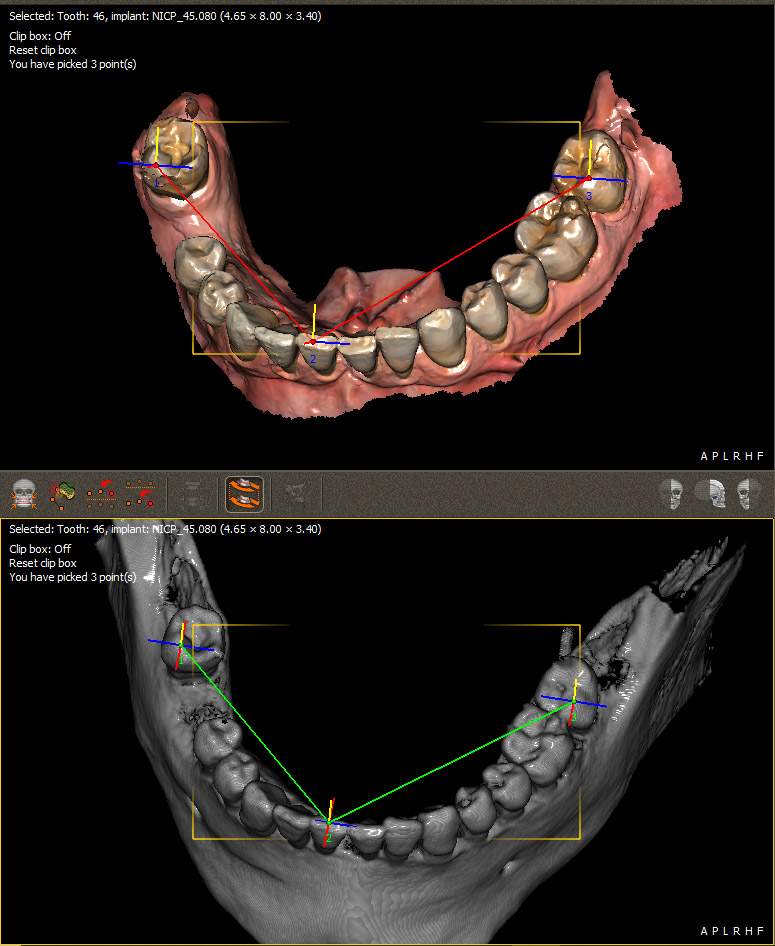
Figure 2 Matching the DICOM and .STL file using QuickVision 3D software
The stages of guided implant planning
The prosthetic project can be entirely digital if a virtual wax-up for edentulous cases is produced. This can be used to display the anatomical and prosthetic project on the same image.
The making of surgical guides therefore requires a combination of three elements:
- DICOM data from the Cone Beam.
- A virtual wax-up of the prosthetic project,
- The patient’s digital impressions.
Planning software can be used to highlight the inferior alveolar nerve.
Once the future prosthesis is in position, it is time to select the position, length and axis of the implants. This can be used to indicate a possible bone graft or sinus lift, and anticipate the prosthetic link method: screw-retained if the implant is on the ideal prosthetic axis, or sealed with an angular pillar if the entrance of the implant screw hole is located on the vestibular side of the future prosthesis.
In the case of several implants, it is also possible to control alignment.
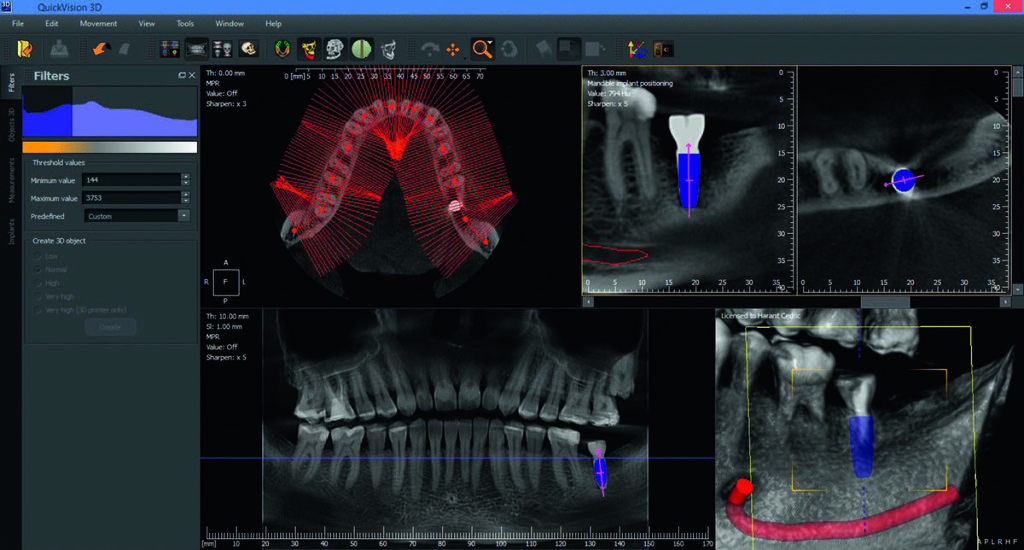
Figure 3 Various sections showing the position of implants on QuickVision 3D planning software
Virtual cylinders are then modelled for the implants above the gingival crest, so there is no interference when inserting the guide into the mouth.
The surgical guide is now ready to be modelled on the .STL file of the edentulous arch, by accurately selecting the supporting surfaces. The guide is created virtually, and a .STL file of this can be exported in order to be printed.
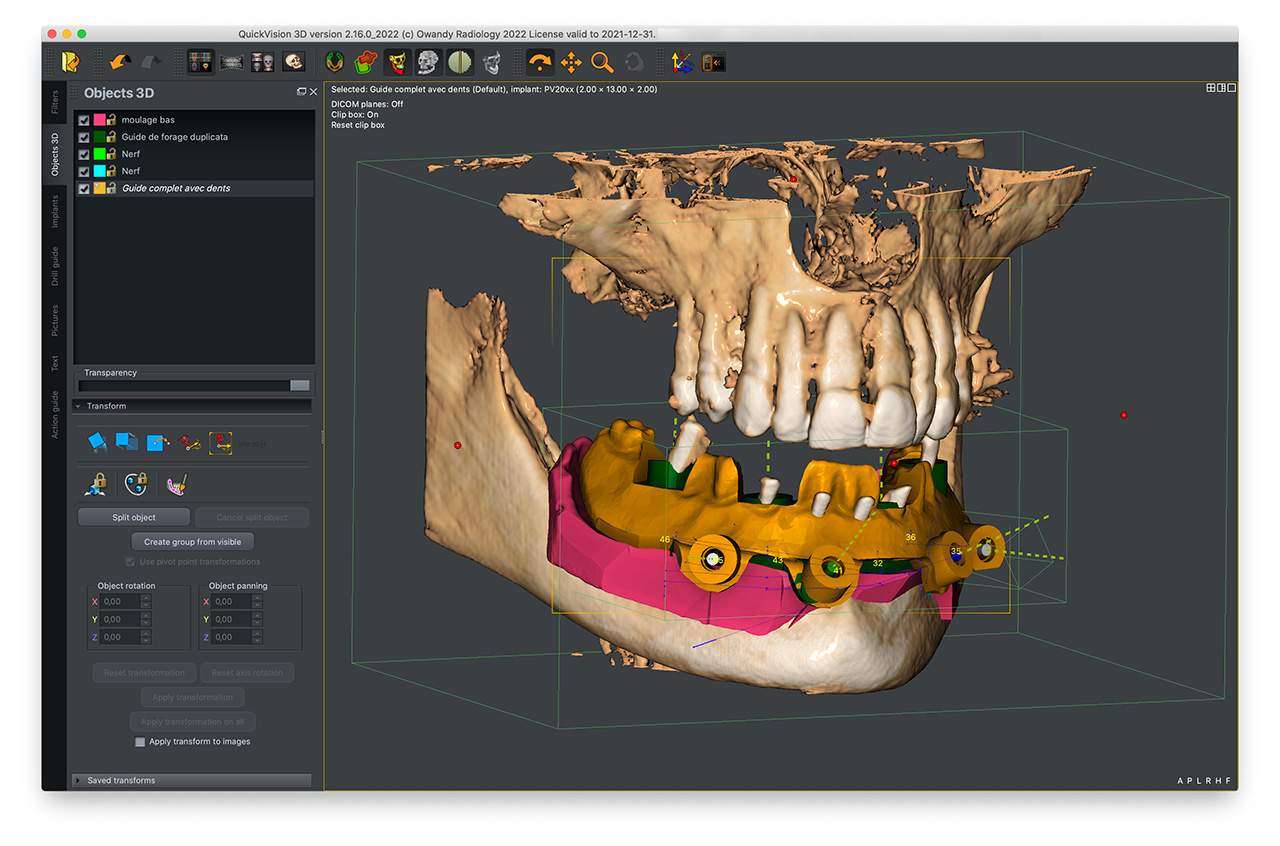
Figure 4 Surgical guide design using QuickVision 3D planning software
Production via 3D printing
A number of additive processes exist, i.e. FDM (Fuse Deposition Modelling) and SLS (Selected Laser Sintering). But the 3D printing technique has experienced a real boom over the last few years, thanks to the SLA (Stereolithographic) technique.
The SLA consists of polymerising a photosensitive resin liquid layer by layer, carried out by a laser beam. This technology combines a high degree of accuracy (print thickness of up to 10μm) with a perfectly smooth surface.
Manufacturers are selling increasingly ergonomically-designed printers that are easier to use, suitable for dental procedures and financially affordable, creating a new market for dental surgeries.
The range of SLA printers in particular is expanding by the day, as exemplified by the case of Form2 by Formlabs.
This company is unique in making available a class I autoclavable biocompatible resin, specially developed for the manufacturing of surgical guides: Dental SG.
Once the guide has been printed, this must be cleaned by immersion in an isopropylic alcohol bath for 20 minutes, before being rinsed and dried, and then post-polymerised in a dedicated UV oven.
After polishing the guide, the titanium cylindrical sleeves find their place via simple friction. This device can then undergo autoclave or gamma ray sterilisation, or cold sterilisation, by plunging it into a chlorhexidine solution.
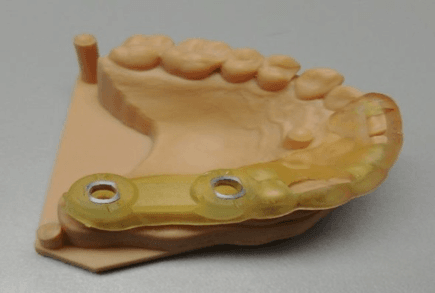
Figure 5 Surgical guide with metal sleeves in place
The various types of surgical guides
There are a number of surgical guides available depending on the surgical technique: adjustment guides with use of the pilot drill only, or fully guided surgical guides.
Depending on the type of guide required, the diameter of its cylinders may vary, as titanium tubes will be inserted.
Implant guides also differ depending on the type of support: tooth, mucosa or bone.
1/ Bone-supported surgical guide
This type of surgical guide requires considerable mucoperiosteum flap-lifting.
2/ Mucosa-supported guide
For full edentulous cases, guide is recommended . Its main advantage lies in the mini-invasive Flapless surgical technique that circumvents the need to use a periosteum flap. However, it does require a certain degree of experience to handle. This guide should be used with an occlusion key, after which a retaining or stabilisation screw (also known as a trans-osseous pin) should be put in place, to keep it firmly in situ with maximum stability.
The bearing surface that the guide sits on is the mucosa, which is a compressible surface up to 3 to 4mm thick. Uneven pressure can cause it to tip and create a deviation in the initial impact point, and therefore in the planned implant angulation.
3/ Tooth-supported guide
It is suitable for anterior or posterior partially tooth-bound edentulism, as well as free-end edentulous cases less than 30mm from the edentulous area. It can also be used for surgeries with or without flaps. Tooth-supported guide is the most accurate of all surgical guides, particularly in the cases of tooth-bound edentulism.
Guided implant surgery software and systems
Currently, there are various software packages and planning systems, including Simplant™ by Dentsply Sirona, the Nobel Guide and Nobel Clinician systems by Nobel Biocare, the Easy Guide system, the CoDiagnostics system by Dental Wings and, lastly, the well-known BlueSky Plan.
The latter was developed by the US company Blue Sky Bio, and is unusual in that it can be downloaded free of charge on the internet.
Thanks to this open access tool, it is possible to virtually model the surgical guide before exporting the .STL file, so as to print it in third party software.
The advantages of guided surgery
Guided implant surgery has made it possible to improve conventional implantology techniques that are restricted in terms of accuracy concerning the choice of implant axis and its proximity to adjacent teeth roots and the various anatomical elements. It can be used to anticipate anatomical obstacles as well as respect the residual bone volume and its suitability for the future prosthetic axis. In conventional implantology, it is mainly the bone configuration of the implant site that guides the drilling, rather than the future prosthetic axis.
Furthermore, the intervention time is much shorter, the surgery reproducible and less invasive, and traceability much simpler.
This benefits both the patient and the practitioner. Flapless surgery reduces stress for the surgeon and the need to improvise during the intervention, as well as making surgical procedures safe by respecting the bone context.
Accurate implant placement in the available bone can help reduce the need for grafts, and even allow implants to be used in complex cases where anatomical limitations had previously prevent treatment.
In addition, this technique improves prosthetic results and simplifies the prosthesis prefabrication process.
The use of guided surgery ensures better post-operative management. It can be used to reduce the risk of pre-operative haemorrhaging along with the risk of infection, and reduce post-operative pain and inflammation, for optimal healing speed.
The surgical guide can also be considered to be a patient communication tool, used to explain procedures and instil confidence through the visualisation of various clinical insights. In time, this tool could offer genuine educational potential.
Difficulties and limitations associated with the technique
Despite the safety that this technology affords the practitioner (albeit on condition of extreme rigour at all stages), it does not preclude the incorporation of anatomical and implantological fundamentals.
The first problem in computer aided surgery lies in the minimal mouth opening, hence the frequent impossibility of placing implants in the posterior section, especially when the guide is present, as it is difficult to introduce the drill into the sleeves. Authors have also noted that the technical sophistication inherent in guided surgery requires a relatively steep learning curve, as it is a highly sensitive and operator-dependent technique and should be adopted with caution.
Benign complications have been reported, particularly discrepancies between simulations and reality.
Accuracy considerations
The search for accuracy is paramount at all stages, similarly requiring precise application of protocols at all stages, i.e. digital planning, surgical guide planning and implementation, implant implementation using guiding cylinders (sleeves) and, lastly, fitting of the prosthesis.
The difference between the actual post-surgical position of the implant and its theoretical position in the implant planning software is determined by measuring three parameters:
- Deviation at the drilling impact point (in mm) or the implant collar level
- Deviation at the apex (in mm)
- Angulation of the implant (in degrees): deviation in the mesio-distal or vestibulo-palatine/lingual direction
Several studies have examined the issue of surgical guide accuracy. This improvement in accuracy being sold to us by surgical guide software and system development companies – is it a myth, or is it real? What’s the truth?
A series of consecutive stages are involved in guided surgery: X-Ray examinations, computer simulation of future implants, and (of course) the production of the stereolithographical guide, its trial, and the guided surgery itself. This would ramp up the number of possible errors, potentially reducing the accuracy of the surgery, knowing that we cannot question the stereolithography process, given that the error rate for SLA does not exceed 0.1%. The use of stereolithographic guides has not shown infallible efficiency in the various studies conducted.
Sarment et al conclude that implant fitting with a guide can reduce discrepancies compared with conventional surgery. In their study, Nickenig et al recognise that the guide is helpful to a degree, but that clinically unacceptable values may result.
Studies by Ozan and Schneider agree on there being little variation in the planning depending on the type of guide support.
The tooth-supported guide is unanimously considered the most accurate, followed by the mucosa-supported guide and, lastly, the bone-supported guide.
It would appear that, regardless of the type of support, the variation in the implant apex position is always greater than that of the collar. Publications show that the average deviation of the implant collar is around 1mm, and that the deviation for the apex is around 1.5mm, with extremely variable standard deviations for both values.
As for angular deviations, the tooth-supported guide accuracy level is considerably higher than that of other guides.
Cost
Despite its innumerable benefits, the use of guided surgery is not yet systematic, and the main obstacle is clearly cost. Often considered high, this cost will have a significant impact on the price of implant treatments. 3D printing in the actual dental surgery itself can help reduce the cost, a course of action being taken by increasing numbers of implantologists and dental surgeons.Obviously, this requires prior training in order to become familiar with the technique of stereolithography, but it is a straightforward and quick formality that has no real influence on the cost of implant treatment.
Conclusion
Digital workflow enables the virtual digital project to be transposed straight into the planning software to generate a surgical guide in the form of a .STL file, and to produce a customised medical device.
The guided implant surgery protocol traditionally reserved for complex cases, for financial reasons, is now increasingly becoming a part of implant surgery treatment plans.
However, the considerable divergence between research findings on accuracy benefits promised by this technique should send a signal that we must not have blind faith in the surgical guide.
This tool is indeed a valuable aid, but it must not diminish the importance of the dental surgeon’s knowledge and experience.
This method is yet to prove itself, especially in terms of accuracy, but it cannot be denied that the principle is revolutionary and could further extend the possibilities of digital and additive technologies, to create dentistry 4.0.